Contributions to Journal Watch are coordinated by Dr Ian Brown, Envoi Pathology, Herston QLD. If you would like to be involved in our Journal Watch, drop us a message via our Contact Page.
Current Edition – 2020
Journal Watch with Drs J Borowsky and C Cooper
Moore M, Lauwers GY, Kumarasinghe MP. Challenges in pathological assessment of endoscopic resections. Diagnostic Histopathology. 2020 Jan 1;26(1):15-21.
This comprehensive and practical review of pathological evaluation of the endoscopic resection specimens, specifically of the oesophagus, stomach and colorectum, has been co-authored by an AGPS member with extensive knowledge and publications in this area. It provides useful tips for handling these specimens, including fixation, cutup and reporting.
Michalski J, Mortellaro M, Lauwers GY, Jiang K. Essential knowledge, precautions and preventive methods required for reaching an accurate intraoperative frozen diagnosis of gastrointestinal cases. Diagnostic Histopathology. 2020 Jan 1;26(1):33-8.
This is an excellent article on frozen sections in GI pathology, a topic rarely covered in the literature. The authors cover the common indications for frozen section, artefacts (and how to avoid them), and discuss common pitfalls in frozen sections. The illustrative cases include discussion of unusual presentations of malignancy, ambiguous features of malignancy, benign mimics of malignancy and malignant mimics of a benign process, and morphology following neoadjuvant therapy.
Dai Y, Zhang Q, Olofson AM, Jhala N, Liu X. Celiac Disease: Updates on Pathology and Differential Diagnosis. Advances in anatomic pathology. 2019 Sep 1;26(5):292-312.
This excellent review covers updates on laboratory testing for coeliac disease (CD), biopsy sparing diagnostic criteria, histopathological features, complications of CD and differential diagnosis. The article covers the histologic spectrum of CD and mimics including enteropathy associated T cell lymphoma (EATL), histology of latent/ potential CD, and evaluation in disease monitoring and treatment response. The Marsh-Oberhuber system and the Corazza-Villanacci score, and methods of enumerating intraepithelial lymphocytes are discussed. The authors include a review of normal histology of the duodenum and jejunum. The sections on pitfalls in diagnosis of CD (which covers technical problems such as poorly oriented or thick sections, inadequate number of biopsies, refractory sprue, collagenous sprue), and neoplastic and other complications, and the differential diagnosis of CD are particularly useful.
Zhang ML, Neyaz A, Patil D, Chen J, Dougan M, Deshpande V. Immune‐related adverse events in the gastrointestinal tract: diagnostic utility of upper gastrointestinal biopsies. Histopathology. 2020 Jan;76(2):233-43.
This paper evaluates gastric and duodenal (in addition to colonic) biopsies to determine histological findings in patients on immune checkpoint inhibitors. The cohort included 39 patients (21 anti-PD1/PD-L1, 17 combination CTLA4 and anti-PD1, 1 CTLA4 only). 29 patients (74%) were clinically determined to have an immune-related adverse (gastrointestinal) event (GI-irAE). Periglandular inflammation and granulomas were the most common finding in gastric biopsies. Duodenal biopsies frequently showed villous blunting, intraepithelial lymphocytosis, granulomas, and neutrophilic activity. Colonic biopsies showed four patterns of injury including acute self-limiting colitis, lymphocytic colitis, collagenous colitis, and apoptosis-only. The most interesting results include A) Histological changes were common in upper gastrointestinal biopsies. Sensitivities of upper and lower GI biopsies for GI-irAE were similar, B).
Histological changes were common in endoscopically normal mucosa, C) Gastric periglandular inflammation and increased mononuclear infiltrate correlated with clinical GI-irAE diagnosis, D) Non-necrotising granulomas were common in the upper GI tract, E) Granulomas and gastric periglandular inflammation are more frequently identified in patients receiving dual therapy, whereas intraepithelial lymphocytosis is typically seen in patients receiving anti‐PD‐1 monotherapy. It is important to note a lack of specificity of histological findings in immune checkpoint associated gastrointestinal damage in trying to discern from a vast array of differential diagnoses.
CLASSIFICATION AND STAGING
Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, Washington KM, Carneiro F, Cree IA, WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020 Jan;76(2):182-8.
This is a great, brief overview of things that have changed in the latest (2019) WHO classification of digestive system entities. It serves more as a prompt of where to look for changes than a comprehensive review of those changes.
Karamchandani DM, Chetty R, King TS, Liu X, Westerhoff M, Yang Z, Yantiss RK, Driman DK. Challenges with colorectal cancer staging: results of an international study. Modern Pathology. 2019 Aug 5:1-1.
This paper details results of a web-based questionnaire distributed amongst an international group of 118 surgical pathologists to gauge practices compared to recommendations set out in the 8th edition of the AJCC cancer staging manual. Many issues were investigated including ones such as T3 and T4a distinction, isolated tumour cells in lymph nodes, acellular mucin deposits in lymph nodes in treatment naïve tumours, staging of neoadjuvantly treated rectal carcinomas, and practices around reporting of tumour budding, intramucosal carcinoma, and mucinous histology. The results found that pathologists adopt highly variable and individualised criteria for reporting when faced with problematic issues not well detailed in the AJCC manual, particularly when limited evidence for AJCC recommendations are given. There was found to be no difference in results based on geographical location, type of pathology practice, or years of practice in the field.
PAEDIATRIC
Tao DH, Vadgama B. Paediatric gastrointestinal pathology: selected topics. Diagnostic Histopathology. 2019 Jul 22.
This is a very nice, though by no means all-encompassing overview of some paediatric gastrointestinal conditions. I particularly liked the comparisons to adult pathology and the summary box of ‘Practice points’ at the end.
Auricchio R, Mandile R, Del Vecchio MR, Scapaticci S, Galatola M, Maglio M, Discepolo V, Miele E, Cielo D, Troncone R, Greco L. Progression of celiac disease in children with antibodies against tissue transglutaminase and normal duodenal architecture. Gastroenterology. 2019 Aug 1;157(2):413-20.
This study investigated the risk factors associated with progression to villous atrophy in children who had positive tissue transglutaminase (tTG) serology but normal duodenal architecture (Marsh 0-1) on initial biopsy. The cohort included a final samples size of 216 children (aged 2 to 18 years old) most followed over 12 years, where symptomatic children were placed on a gluten free diet (GFD) after diagnosis, and serology was taken every 6 months and small bowel biopsy every 2 years. 15% developed villous atrophy (cumulative incidence at 12 years 43%) and 32% no longer tested positive for tTG. Baseline factors able to predict 80% of children who developed villous atrophy included numbers of gamma-delta intraepithelial lymphocytes on initial biopsy, age, and homozygosity for HLA DQB1*02.
APPENDIX
Lowes H, Rowaiye B, Carr NJ, Shepherd NA. Complicated appendiceal diverticulosis versus low‐grade appendiceal mucinous neoplasms: a major diagnostic dilemma. Histopathology. 2019 Oct;75(4):478-85.
The main aim of this paper was to investigate histological clues to assist pathologists in differentiating complicated diverticular disease of the appendix (ADD) particularly when associated with a mucous cyst from low grade appendiceal mucinous neoplasms (LAMN). The authors assessed 74 cases of complicated ADD at two specialist centres, as well as a case-control study of 30 ADD and LAMN cases. The following features were determined to best differentiate between the two entities:
Horvath BA, Maryamchik E, Miller GC, Brown IS, Setia N, Mattia AR, Lamps L, Lauwers GY, Rosenberg E, Misdraji J. Actinomyces in Crohn’s‐like appendicitis. Histopathology. 2019 Oct;75(4):486-95.
This study evaluated actinomyces found in appendiceal specimens. Authors investigated 20 cases of appendicitis with Crohn’s-like histological features that were due to Actinomyces and compared features to 60 control cases (22 known Crohn’s disease, 34 interval appendicectomies, and 4 idiopathic granulomatous appendicitis). Features to prompt a higher level of suspicion of actinomyces included greater degrees of lymphoid hyperplasia, transmural lymphoid aggregates, and fibrosis. The authors recommend submission of entire appendix if suspicious as actinomyces were often only found in 1-2 blocks. Gomori methenamine silver stain was more reliable in staining actinomyces than Brown-Hopps. Authors also reviewed an additional 100 consecutive routine appendicectomies and found actinomyces in only 2%, surmising that they are not incidental/bystander bacteria.
IMMUNOHISTOCHEMISTRY
Hot Topic – SATB2
Special AT-rich sequence-binding protein 2 (SATB2) is a protein encoded by the SATB2 gene. It is involved in transcriptional regulation and chromatin remodeling and mainly expressed in epithelial cell nuclei of colon and rectum, as well as brain neurons. Several papers of interest detailed below look at SATB2 immunohistochemical staining in gastrointestinal entities. A quick summary table of the main findings is provided here.

Ma C, Henn P, Miller C, Herbst C, Hartman DJ, Pai RK. Loss of SATB2 Expression Is a Biomarker of Inflammatory Bowel Disease–associated Colorectal Dysplasia and Adenocarcinoma. The American journal of surgical pathology. 2019 Oct 1;43(10):1314-22.
The authors investigated immunohistochemical expression of SATB2 in IBD-associated colorectal dysplasia and carcinoma. Their cohort included
- 37 cases of IBD-associated dysplasia (15 low-grade and 22 high-grade dysplasia) with a reference cohort of 50 IBD cases without dysplasia, 20 conventional adenomas, 20 sessile serrated lesions
- 36 cases of IBD-associated carcinoma with a reference cohort of 343 sporadic colorectal carcinomas.
SATB2 expression was either completely lost or weak and focal (H score ≤10) in 41% of cases of IBD-associated dysplasia, while none (0%) of their reference cohort showed loss of expression. Loss of expression was more frequent in high-grade dysplasia and non-polypoid visible dysplasia.
SATB2 expression was lost in 67% of IBD-associated colorectal carcinomas compared with 14% of sporadic colorectal carcinomas (p<0.001). No difference was found between the two carcinoma groups with CDX2 expression. The authors discussed the implications for using SATB2 as a marker of colorectal origin in an IBD setting and the importance of CDX2 in this scenario. Despite prior literature indicating a worse prognosis for both sporadic and IBD-associated colorectal carcinomas associated with SATB2 loss, this paper could not identify any differences in tumour stage or patient survival based on SATB2 expression pattern.
Meagher NS, Wang L, Rambau PF, Intermaggio MP, Huntsman DG, Wilkens LR, El-Bahrawy MA, Ness RB, Odunsi K, Steed H, Herpel E. A combination of the immunohistochemical markers CK7 and SATB2 is highly sensitive and specific for distinguishing primary ovarian mucinous tumors from colorectal and appendiceal metastases. Modern Pathology. 2019 Dec;32(12):1834-46.
This paper tests the utility of adding SATB2 to the traditional immunostain panel (CK7, CK20, CDX2, and PAX8) to distinguish primary ovarian mucinous tumors from metastatic gastrointestinal neoplasms. Their cohort included a test cohort (full panel applied)
- 155 ovarian mucinous tumours (105 mucinous carcinomas, 50 mucinous borderline tumours)
- 230 primary lower gastrointestinal tract neoplasms (123 colorectal adenocarcinoma, 107 appendiceal neoplasm including 39 goblet cell carcinoma, 24 LAMNs, 20 carcinoids, 12 high grade appendiceal mucinous neoplasms, and 12 non-mucinous adenocarcinomas)And an international validation cohort (PAX8 and SATB2 only)
205 ovarian mucinous tumour (159 invasive and 46 borderline) as well as 2671 ovarian carcinomas of other histiotypes.
The most effective combination was the two marker combination of CK7 and SATB2 which was able to distinguish lower gastrointestinal from ovarian primary mucinous tumours with 95% accuracy. This combination outperformed the standard panel of CK7, CK20 and CDX2 (87.5%). Accuracy of SATB2 was confirmed in the validation cohort (91.5%). The inclusion of PAX8 was able to aid in the distinction from ovarian tumours of histiotypes other than mucinous.
Bellizzi AM. SATB2 in neuroendocrine neoplasms: strong expression is restricted to well‐differentiated tumours of lower gastrointestinal tract origin and is most frequent in Merkel cell carcinoma among poorly differentiated carcinomas. Histopathology. 2020 Jan;76(2):251-64.
This study investigated the role of SATB2 in assigning site of origin in neuroendocrine epithelial neoplasms. The cohort included 317 well-differentiated neuroendocrine tumours (NETs) and 79 poorly differentiated neuroendocrine carcinomas (NECs) from gastrointestinal and non-gastrointestinal sites. SATB2 expression was highly sensitive (86%) and specific (93%) for lower GI tract origin among NETs and strong SATB2 expression was fairly specific for Merkel cell carcinoma among NECs.
In addition, the following were of interest:
Ritterhouse LL, Wu EY, Kim WG, Dillon DA, Hirsch MS, Sholl LM, Agoston AT, Setia N, Lauwers GY, Park DY, Srivastava A. Loss of SMAD4 protein expression in gastrointestinal and extra‐gastrointestinal carcinomas. Histopathology. 2019 Oct;75(4):546-51.
The main finding of this paper revolved around SMAD4 expression in CK7 positive tumours in the assessment of carcinomas of unknown primary site. Authors evaluated SMAD4 immunohistochemical expression in 1210 cases and found that whilst SMAD4 loss has generally been interpreted to suggest pancreaticobiliary or colonic origin (58% showed loss), it was also lost in a small proportion of other CK7 positive tumours including breast (<5%), lung (10%), oesophageal (<5%), and gastric carcinomas(<5%). Authors also provide results on staining in several CK7 negative tumours.
Liu C, Ghayouri M, Brown IS. Immunohistochemistry and special stains in gastrointestinal pathology practice. Diagnostic Histopathology. 2020 Jan 1;26(1):22-32.
This review with 2 AGPS members as co-authors is a very useful practical review of both special stains and immunohistochemistry. This review includes interpretation of commonly used immunohistochemistry such as MMR in GI cancers, use of SATB2 in IBD related dysplasia, and SDHA and SDHB immunohistochemistry in GISTs. Other sections including indications for H. pylori IHC, pitfalls in CMV IHC, and use of CD3/ CD8 in refractory coeliac disease are also valuable.
Yozu M, Kem M, Cenaj O, Mino‐Kenudson M, Odze RD, Misdraji J. Loss of expression of MLH1 in non‐dysplastic crypts is a harbinger of neoplastic progression in sessile serrated adenomas/polyps. Histopathology. 2019 Sep;75(3):376-84.
158 without dysplasia (SSA), 219 with dysplasia (SSAD), and 23 with invasive adenocarcinoma (SSAC). 18% showed loss of MLH1 in non-dysplastic crypts including 7% of SSAs, 22% SSADs, and 52% SSAC. Loss of MLH1 in non-dysplastic crypts was more frequent in cases with MLH1 loss in dysplasia and more common adjacent to dysplastic crypts showing MLH1 loss. The authors postulate that MLH1 loss in non-dysplastic crypts may precede progression and indicate an advanced polyp. Routine staining of MLH1 in serrated polyps without morphological dysplasia is however not recommended until prospective studies are available.
POLYPOSIS
Borowsky J, Setia N, Rosty C, Conrad R, Susman R, Misdraji J, Hart J, Lauwers GY, Brown IS. Spectrum of gastrointestinal tract pathology in a multicenter cohort of 43 Cowden syndrome patients. Modern Pathology. 2019 Dec;32(12):1814-22.
- This paper aims to evaluate and raise pathologist awareness of the characteristic admixture of lesions seen in the gastrointestinal tract of patients with Cowden patients. The international cohort included 43 patients who underwent a total of 199 endoscopic procedures. The paper details several important parameters that may help pathologists raise the possibility of Cowden syndrome based on histological findings:
- The spectrum of lesions. The most common lesions found are detailed here:
- The characteristic diversity of stromal components (lymphoid, lipomatous, ganglioneuromatous, fibrous-rich) in hamartomatous polyps in Cowden syndrome. More than half (55%) of patients in this series had hamartomatous polyps with two or more stromal components. Of interest S100 immunostain highlighted a neuromatous element in a subset of hamartomatous polyps with fibrous rich stroma. CD34 immunostain highlighted fibrous –rich stroma.
- Importantly, an admixture of polyps was present in many patients. Hamartomatous polyps were associated with serrated polyps in 48% and conventional adenomas in 43%. All patients with glycogenic acanthosis had colorectal hamartomatous polyps on colonoscopy.
MOLECULAR
Pai RK, Bettington M, Srivastava A, Rosty C. An update on the morphology and molecular pathology of serrated colorectal polyps and associated carcinomas. Modern Pathology. 2019 Oct;32(10):1390-415.
This article (co-authored by 2 AGPS members who have published extensively on this topic) is a comprehensive review of serrated polyps. The article includes classical histopathological features, revised nomenclature (as published in the current WHO), discussion of the (often difficult) topic of dysplasia in serrated polyps, use of MLH1 immunohistochemistry in dysplasia, and traditional serrated adenomas. The discussion of controversial issues in serrated polyps is particularly interesting and reflects problems encountered in daily reporting. The authors also discuss the molecular features of these polyps, risk of neoplasia, serrated polyposis syndrome including updated diagnostic criteria, and serrated pathway associated carcinomas.
LIVER
Volume 6 of Seminars in Diagnostic Pathology 2019 was dedicated to non-neoplastic liver disease. All reviews were a worthwhile read. Only a few are represented below:
Kwong S, Meyerson C, Zheng W, Kassardjian A, Stanzione N, Zhang K, Wang HL. Acute hepatitis and acute liver failure: Pathologic diagnosis and differential diagnosis. InSeminars in diagnostic pathology 2019 Jul 24. WB Saunders.
This review covers general features of acute hepatitis, specific aetiologies of acute hepatitis and their potentially unique histological findings, a discussion of the distinction between collapse and cirrhosis (sometimes tricky in practice and well-illustrated in this article including the use and limitations of special stains) and limitations of histology in this clinical setting. This article also covers non-necrotic acute liver failure, with histological features of microvesicular steatosis related to mitochondrial dysfunction, and the role of molecular testing.
Guindi M. Wilson disease. InSeminars in diagnostic pathology 2019 Jul 25. WB Saunders.
This article comprehensively reviews copper metabolism, genetics, clinical diagnosis and use of other ancillary tests such as serum ceruloplasmin and urinary copper excretion in diagnosis of WD. It discusses indication for liver biopsy, range of histological features (including steatosis, steatohepatitis, chronic hepatitis and acute hepatitis), histochemical stains (including sensitivity, specificity and practicalities), and copper quantitation including practice tips. Genetic testing is discussed.
Lee HE, Zhang L. Immunoglobulin G4-related hepatobiliary disease. InSeminars in diagnostic pathology 2019 Jul 24. WB Saunders.
This article discussed the diagnostic criteria and differential diagnosis of IgG4- sclerosing cholangitis, which has been relatively well characterized in the literature. It also discusses the less well characterized liver manifestations of IgG4 related disease (IgG4—RD) including IgG4-hepatopathy and IgG4-autoimmune hepatitis (AIH). IgG4 hepatopathy has several patterns of injury and encompasses hepatic injury primarily and secondarily related to Type 1 AIP or IgG4 sclerosing cholangitis. IgG4- AIH shows histological features of AIH but with >10 IgG4+ plasma cells/hpf- it is currently unclear whether this represents a distinct entity or a subtype of AIH with increased numbers of IgG4+ plasma cells. Potential histological mimics seen in liver biopsy including classic AIH, syphilis and lymphoma are considered. The section on the use and interpretation of IgG4 and IgG immunohistochemistry in liver pathology is a very useful practice tip.
Zen Y, Yeh MM. Checkpoint inhibitor-induced liver injury: A novel form of liver disease emerging in the era of cancer immunotherapy. InSeminars in diagnostic pathology 2019 Jul 24. WB Saunders.
This paper discussed Immune related adverse events (irAE) in the liver, which have been seen since 2011 when ipilumimab was first approved for treatment of metastatic melanoma, and which are seen with all types of checkpoint inhibitors, although most of the literature relates to ipilumimab and nivolumab with only limited information available for second generation drugs. The authors discuss timing, frequency, grade of liver injury as well as current indications for biopsy and treatment. They review the patterns of injury seen in liver biopsies, with the commonest panlobular hepatitis (70%), followed by isolated central zonal necrosis (20%), with less common patterns of granulomatous hepatitis (5%) and the remaining cases showing NRH or steatohepatitis (5%). The authors also compare histological features and immunophenotype of the lymphocytic infiltrate with idiosyncratic drug induced liver injury and autoimmune hepatitis, which seem to have distinct features. The authors also discuss sclerosing cholangitis, a less common form of irAE. Immune checkpoint therapy can also unmask a preexisting/ undiagnosed liver disease. An interesting article with practical illustrations.
LYMPHOMA
van Vliet C, Spagnolo DV. T-and NK-cell lymphoproliferative disorders of the gastrointestinal tract: review and update. Pathology. 2019 Nov 11.
This is a worthwhile review to read on the topic of gastrointestinal T and NK cell lymphomas and lymphoproliferative disorders, particularly for its practical insights on what is required clinically to make a diagnosis especially for the lymphoproliferative conditions. The pitfalls and pearls sections for each topic are great if you have limited reading time.
GALLBLADDER
Akki AS, Zhang W, Tanaka KE, Chung SM, Liu Q, Panarelli NC. Systematic Selective Sampling of Cholecystectomy Specimens Is Adequate to Detect Incidental Gallbladder Adenocarcinoma. The American journal of surgical pathology. 2019 Dec 1;43(12):1668-73.
This paper examines the possibility of a standardised protocol for gallbladder sampling procedures in routine cholecystectomy specimens where initial routine sections reveal intestinal metaplasia (IM), low grade dysplasia (LGD), or high grade dysplasia (HGD). The authors performed a 26-month retrospective analysis followed by a 24-month prospective validation study. Their cohort included 87 cases where routine sections (cystic duct and 2 random longitudinal) of gallbladders from a series of routine cholecystectomies revealed IM or dysplasia, including 48 from the retrospective series (of 4059 cholecystectomies) and 39 from the prospective series (of 3133 cholecystectomies).
In the retrospective analysis, the 48 cases were further examined using their laboratories protocol at the time (5 random sections for cases with IM, submission of entire specimen for cases with dysplasia). Sixteen (33%) of cases had additional findings on further sections as per table:
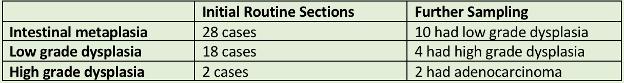
For the prospective analysis, the authors tested their proposed protocol on the 39 identified cases following findings on initial routine sections. To test the validity of their protocol they additionally entirely submitted all cases showing dysplasia on routine section. No further adverse findings were seen on those entirely submitted sections compared to protocol sections alone.
Proposed Protocol
- Sampling that includes 2 to 3 random sections and 1 section of the cystic duct is adequate in most cases; gross abnormalities should be entirely submitted “up-front”
- Finding isolated IM in routine sections does not warrant further sampling
- In cases with LGD, 1 additional section per centimeter of the greatest dimension of the gallbladder is adequate to detect HGD
- Cases with HGD should be entirely submitted for cancer detection and accurate staging
INFLAMMATORY BOWEL DISEASE
Hissong E, Chen Z, Yantiss RK. Cytomegalovirus reactivation in inflammatory bowel disease: an uncommon occurrence related to corticosteroid dependence. Modern Pathology. 2019 Aug;32(8):1210-6.
This paper sets out to evaluate whether rates of cytomegalovirus infection in inflammatory bowel disease (IBD) biopsy specimens has decreased with the reduced use of steroids and increased immunomodulatory therapy for IBD in recent times. Their cohort included 268 patients with biopsies for severe IBD flares, divided into 135 corticosteroid-dependent patients (maintained with corticosteroids) and 133 corticosteroid-independent patients (no steroids within 6 months of colonoscopy). The majority of corticosteroid-dependent patients were sourced from an earlier time frame (2002-2009) than the corticosteroid-independent patients (2009-2017). Biopsies were reviewed for viral inclusions and stained for cytomegalovirus immunohistochemistry. Cytomegalovirus was only detected in steroid-dependent patients and many of these (69%) were from the earlier time period (2002-2009). This article brings into question routine immunohistochemical testing for cytomegalovirus in all IBD patients with medically refractory disease.
Shah A, Walker M, Burger D, Martin N, von Wulffen M, Koloski N, Jones M, Talley NJ, Holtmann GJ. Link between celiac disease and inflammatory bowel disease. Journal of clinical gastroenterology. 2019 Aug 1;53(7):514-22.
A systematic review to investigate the link between coeliac disease and inflammatory bowel disease (IBD). 27 studies which included 41,482 adult IBD patients (20,357 Crohn’s disease (CD), 19,791 Ulcerative colitis (UC) and 459 coeliac disease). Results were consistent with coeliac disease patients being at increased risk of IBD and vice versa (to a lesser degree), with prevalence rates increased above respective reference population rates (11.10 and 2.23 respectively). No differences in rates was noted between CD and UC. Authors refer to Festen et al who identified 4 shared risk loci between coeliac disease and CD in GWAS.


